Abstract

Background
Allogeneic hematopoietic stem cell transplantation (SCT) is the only established curative treatment option for patients with sickle cell disease (SCD). Transplantations with an HLA-identical matched sibling donor (MSD) have resulted in excellent disease-free survival of >90% and overall survival (OS) of >95%. However, lack of HLA-identical siblings is a limiting factor. The chance of finding a potential matched unrelated donor is low for patients with a non-Western ethnic background (< 20%). Haploidentical related donors are a promising pool of donors potentially extending SCT as a curative treatment to a larger group of SCD patients with no other meaningful treatment options. Myeloablative conditioning regimens (MAC) are not recommended for adult SCD patients, as cumulative SCD-related organ damage renders these patients susceptible to increased toxicity and higher risk of transplant-related mortality. Using reduced-intensity conditioning (RIC) or non-myeloablative conditioning (NMC) in both adult and pediatric patients has resulted in decreased transplant-related toxicity and mortality. However, while successful in hematologic malignancies, NMC has been associated with significant risk of graft failure in hemoglobinopathies. In the present study, we aimed to systematically review (1) the outcomes of haploidentical SCT (Haplo-SCT), (2) the effects of conditioning intensity and modes of T-cell depletion on Haplo-SCT outcomes and (3) comparative outcomes between matched sibling donor SCT (MSD-SCT) and Haplo-SCT in selected studies.
Methods
A comprehensive search was performed in MEDLINE/PubMed and Embase up to May 2021. Data was extracted by two reviewers independently and the Newcastle-Ottawa Quality Assessment Scale was used to assess the quality of the studies. Only studies reporting at least one of the outcomes: graft failure, OS, transplant-related mortality, and acute/chronic graft-versus-host disease (GvHD) were included. Fourteen studies met the inclusion criteria. To have an overview of the results of Haplo-SCT, we divided the included studies in four groups according to the conditioning intensity (MAC versus NMC/RIC) and the T-cell depletion method (in vivo (post-transplant cyclophosphamide (PTCy)) vs. in vitro).
Results
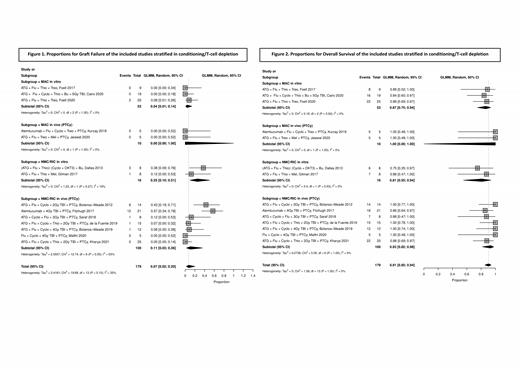
All included studies were observational cohort studies. A subgroup meta-analysis of the results of Haplo-SCT showed relatively low overall pooled proportions of graft failure (7%, 95% CI: 2 - 20), acute (4%, 95% CI: 2 - 12) and chronic (11%, 95% CI: 7 - 16) GvHD. Overall survival was high (91%, 95% CI: 85 - 94). Graft failure in MAC-in vitro, MAC-in vivo, NMC/RIC-in vitro and NMC/RIC-in vivo groups was 4% (95% CI: 1 - 14), 0% (95% CI: 0 - 100), 25% (95% CI: 10 - 51) and 11% (95% CI: 3 - 36) respectively (Figure 1). OS was 100% and 93% for MAC and NMC/RIC groups with PTCy (in vivo T-cell depletion) respectively. In patients with in vitro T-cell depletion, OS was 87% and 81% in MAC and NMC/RIC groups respectively (Figure 2). Based on a comparative meta-analysis of the three studies that included both haploidentical and MSD transplantation, graft failure was significantly higher in the haploidentical group than in the MSD group (odds ratio 5.3, 95% CI: 1.0 - 27.6). Overall survival, transplant-related mortality and acute/chronic GvHD were not significantly different between the groups.
Conclusions
This systematic review shows that modifications in the intensity of the conditioning regimen and improved T-cell depletion approaches in Haplo-SCT in SCD have led to reduced transplantation-related toxicity while keeping graft failure rates low. Both in vitro and in vivo (PTCy) T-cell depletions result in very low transplantation-related mortality, though in vitro T-cell depletion is associated with a higher incidence of viral reactivations and other infectious complications.
Haploidentical stem cell transplantation is becoming a viable alternative curative option for SCD, extending the availability of allogeneic SCT as a treatment option to many more transplant eligible SCD patients. Novel immunosuppression (immunoablation) and improvement in supportive care have allowed the use of RIC or NMC regimens, resulting in low risk of transplantation-related complications and improvement in engraftment rates.
Biemond: Global Blood Therapeutics: Honoraria, Research Funding, Speakers Bureau; Novartis: Honoraria, Research Funding, Speakers Bureau; CSL Behring: Honoraria; Sanquin: Research Funding; Novo Nordisk: Honoraria; Celgene: Honoraria. Nur: Celgene: Speakers Bureau; Roche: Speakers Bureau; Novartis: Research Funding, Speakers Bureau.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal